In an operation where inhalation anesthetics are used, some amount of those anesthetics are dispersed into the operation room. When that happens, medical staff may be exposed to trace amounts of these gases. While a single instance of exposure is likely negligible, over the course of a multi-decade career, more serious issues can emerge.
Research has not revealed a direct link between chronic exposure to low levels of anesthetic gases and specific long-term health conditions. However, hazards have not been definitively ruled out. A study by Mierdl et al. studied the presence of common inhalation anesthetics in surgeons, anesthesiologists and perfusionists, both before and after a surgery. The study found that all three roles had elevated levels of these gases after the surgery concluded. Surgeons and anesthesiologists showed the highest levels of concentration—up to 9 ppm for some gases [1].
Other studies have suggested a correlation between chronic exposure to inhalation anesthetics and reproductive toxicity. A study by Corbett et al. looked at birth defects in the children of nurse anesthetists. The children of those who worked during pregnancy had birth defects in 16.4% of cases, compared to 5.7% of those whose mothers did not work during pregnancy [2]. A more recent study by Jevtovic-Todorovic et al. exposed rats to varying levels of nitrous oxide and then tested the effects on a subset of neurons. The study found that high levels of short-term nitrous oxide exposure led to neuronal injury in adult rats. Long-term exposure resulted in neuron death [3]. In an article in Best Practice & Research Clinical Anesthesiology by Anton Burm, the author notes that these conditions were found when rats were exposed to concentrations of 1,000 ppm or higher, which can occur in poorly ventilated operating rooms [4].
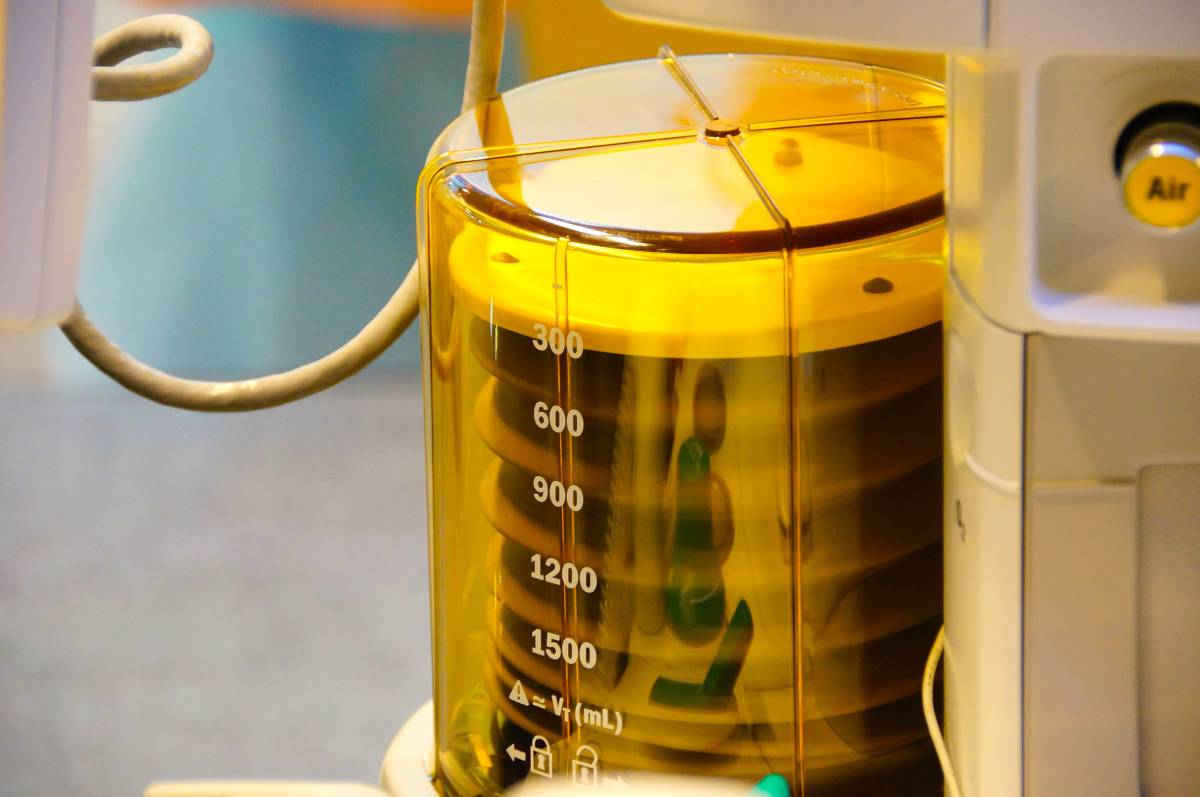
Most studies suggest that, while chronic exposure to waste anesthetic gases may not cause immediate damage, it is still best to mitigate exposure. The Occupational Safety and Health Administration notes that, until the 1970s, it was common practice to exhaust waste gas using the expiratory valve, which often directs into the face of the anesthesia provider. Today, efficient scavenging systems capture these gases directly from the valve, significantly lowering exposure [5].
However, exposure still occurs, and frequent assessments are a useful way of determining the levels of exposure in an operating room. OSHA suggests sampling a known quantity of air and analyzing the levels of particulates using a flame-ionization detector [6]. A study by Sakhvidi et al. found that solid-phase microextraction (SPME) samplers can be a useful tool in determining occupational exposure. The study found it to be as reliable as the OSHA method and particularly useful in the operating room [7].
Short-term exposure to dispersed inhalation anesthetics likely has little permanent impact on subjects. However, chronic exposure has been correlated with certain health conditions. While there has been no conclusive evidence that exposure to waste anesthetic gases results in adverse health effects, most of the research on the topic concludes that healthcare professionals should avoid long-term exposure. Proper ventilation and testing were cited as two of the most common ways to assess and prevent exposure.
References
[1] Mierdl, S., et al. “Occupational Exposure to Inhalational Anesthetics during Cardiac Surgery on Cardiopulmonary Bypass.” The Annals of Thoracic Surgery, vol. 75, no. 6, 2003, pp. 1924–1927., doi:10.1016/s0003-4975(03)00003-1.
[2] Corbett, T. H., et al. “Birth Defects among Children of Nurse-Anesthetists.” Anesthesiology, vol. 41, no. 4, 1974, pp. 321–344., doi:10.1097/00000542-197410000-00005.
[3] Jevtovic-Todorovic, V., et al. “Prolonged Exposure to Inhalational Anesthetic Nitrous Oxide Kills Neurons in Adult Rat Brain.” Neuroscience, vol. 122, no. 3, 2003, pp. 609–616., doi:10.1016/j.neuroscience.2003.07.012.
[4] Burm, Anton G. l. “Occupational Hazards of Inhalational Anaesthetics.” Best Practice & Research Clinical Anaesthesiology, vol. 17, no. 1, 2003, pp. 147–161., doi:10.1053/bean.2003.0271.
[5] OSHA Directorate of Technical Support and Emergency Management. “Anesthetic Gases: Guidelines for Workplace Exposures.” Waste Anesthetic Gases, Occupational Safety and Health Administration, 18 May 2000, www.osha.gov/dts/osta/anestheticgases/.
[6] “Sampling and Analytical Methods: Enflurane Halothane Isoflurane – (Organic Method #103).” Sampling and Analytical Methods, Occupational Safety and Health Administration, www.osha.gov/dts/sltc/methods/organic/org103/org103.html.
[7] Sakhvidi, M. J. Z., et al. “Field Application of SPME as a Novel Tool for Occupational Exposure Assessment with Inhalational Anesthetics.” Environmental Monitoring and Assessment, vol. 184, no. 11, 2011, pp. 6483–6490., doi:10.1007/s10661-011-2434-7.