Preoperative blood transfusion is a component of perioperative management aimed at optimizing hemoglobin levels, improving oxygen delivery, and minimizing perioperative morbidity and mortality, particularly in high-risk surgical patients. The decision to transfuse blood before surgery is complex and must be individualized based on patient factors such as underlying anemia, comorbid conditions, type of surgical procedure, and anticipated blood loss. There is no universal hemoglobin threshold for transfusion; however, guidelines generally recommend considering transfusion when hemoglobin levels fall below 7-8 g/dL in stable patients and higher thresholds in patients with cardiovascular disease or active bleeding (1).
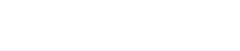
Patients undergoing procedures with a high risk of blood loss, such as orthopedic or cardiovascular surgery, may benefit from preoperative transfusion if they have moderate to severe anemia. In particular, the use of preoperative blood transfusion in neurosurgical procedures such as craniotomy for tumor resection has shown relevance due to the potential for sudden and significant blood loss during surgery. Aziz et al (2025) highlighted that preoperative identification of patients at risk allows for proactive transfusion strategies that improve intraoperative hemodynamics and postoperative outcomes (1).
Preoperative autologous blood donation (PABD) has been explored as a strategy to reduce the need for allogeneic transfusion. In a study focused on spine surgery, Qi et al (2024) demonstrated that PABD can effectively reduce donor blood exposure while maintaining perioperative safety, especially in elective surgery (2). However, PABD requires adequate planning and patient stability, making it unsuitable for emergency or urgent surgery. In addition, the limited shelf life and logistical challenges associated with autologous blood storage present barriers to its broader implementation.
Evaluation of coagulation parameters, such as international normalized ratio (INR) and activated partial thromboplastin time (aPTT), is often part of the preoperative evaluation to predict bleeding risk. However, these parameters do not reliably predict the need for plasma transfusion in all settings. D’Albuquerque et al (2025) reported that INR and aPTT were poor predictors of actual plasma transfusion requirements in liver transplantation, suggesting that clinical judgment and comprehensive assessment remain essential (3).
Patient Blood Management (PBM) programs are increasingly emphasized to optimize transfusion practices. These programs include identification and correction of anemia before surgery, minimization of blood loss during surgery, and use of restrictive transfusion strategies. Barkeji et al (2024) analyzed the utility of routine preoperative “group and save” testing and emphasized that many low-risk surgeries may not require routine pretransfusion testing unless patients have specific risk factors for bleeding or transfusion (4). Such stratification reduces unnecessary laboratory testing and conserves resources without compromising patient safety.
Overall, indications for preoperative blood transfusion are based on clinical judgment, patient-specific risk profiles, and the nature of the surgical procedure. Evidence suggests that targeted transfusion strategies and integration of PBM principles can optimize outcomes while reducing exposure to allogeneic blood products. However, ongoing research is essential to refine transfusion thresholds, improve patient stratification tools, and develop individualized management protocols tailored to surgical risk and comorbidities.
References
- Aziz N, Waqar U, Bukhari MM, Uzair M, Ahmed S, Naz H, Shamim MS. Blood transfusions in craniotomy for tumor resection: Incidence, risk factors, and outcomes. J Clin Neurosci. 2025 Feb;132:111009. doi: 10.1016/j.jocn.2024.111009. Epub 2024 Dec 27. PMID: 39732040.
- Qi J, Hu Y, Niu X, Dong Y, Zhang X, Xu N, Chen Z, Li W, Tian Y, Sun C. Efficacy of Preoperative Autologous Blood Donation for Surgical Treatment of Thoracic Spinal Stenosis: A Propensity-Matched Cohort Study. Orthop Surg. 2024 Dec;16(12):3068-3077. doi: 10.1111/os.14249. Epub 2024 Oct 2. PMID: 39356001; PMCID: PMC11967701.
- Marinho DS, Rocha Filho JA, Figueira ERR, et al. International normalized ratio and activated partial thromboplastin time do not predict plasma transfusion in liver transplantation. Arq Bras Cir Dig. 2025;37:e1855. doi:10.1590/0102-6720202400061e1855
- O’Leary L, Sherwood WB, Fadel MG, Barkeji M. Assessment of routine pre-operative group and save testing in patients undergoing cholecystectomy: a retrospective cohort study. NIHR Open Res. 2024 Oct 23;4:17. doi: 10.3310/nihropenres.13543.2. PMID: 39473540; PMCID: PMC11519620.